Regulation of Respiration – The regulation of normal lung function
Introduction
Spontaneous respiration is produced by the rhythmic discharge of motor neurons that innervate the respiratory muscles. This discharge is totally dependent on nerve impulses from the brain; breathing stops if the spinal cord is transected above the origin of the phrenic nerves.
NEURAL CONTROL OF BREATHING CONTROL SYSTEMS
Two separate neural mechanisms regulate respiration. One is responsible for a voluntary control and the other for automatic control. The voluntary system is located in the cerebral cortex and sends impulses to the respiratory motor neurons via the corticospinal tracts. The automatic system is driven by a group of pacemaker cells in the medulla.
Medullary systems
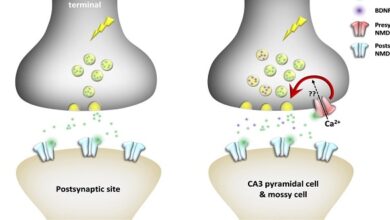
The main components of the respiratory control pattern generator responsible for automatic respiration are located in the medulla. Rhythmic respiration is initiated by a small group of synaptically coupled pacemaker cells in the pre-Bötzinger complex (pre-BÖTC) on either side of the medulla between the nucleus ambiguous and the lateral reticular nucleus. These neurons discharge rhythmically, and they produce rhythmic discharges in phrenic motor neurons that are abolished by sections between the pre-Bötzinger complex and these motor neurons. They also contact the hypoglossal nuclei, and the tongue is involved in the regulation of airway resistance
Neurons in the pre-Bötzinger complex discharge rhythmically in brain slice preparations in vitro, and if the slices become hypoxic, discharge changes to one associated with gasping. The addition of cadmium to the slices causes occasional sigh-like discharge patterns. There are NK1 receptors and μ-opioid receptors on these neurons, and, in vivo, substance P stimulates and opioids inhibit respiration. Depression of respiration is a side effect that limits the use of opioids in the treatment of pain. However, it is now known that 5HT4 receptors are present in the pre-Bötzinger complex and treatment with 5HT4 agonists blocks the inhibitory effect of opiates on respiration in experimental animals, without inhibiting their analgesic effect.
Pontine & vagal influences
Although the rhythmic discharge of medullary neurons concerned with respiration is spontaneous, it is modified by neurons in the pons and afferents in the vagus from receptors in the airways and lungs. An area is known as the pneumatic center in the medial parabrachial and Kölliker–Fuse nuclei of the dorsolateral pons contains neurons active during inspiration and neurons active during expiration. When this area is damaged, respiration becomes slower and tidal volume greater, and when the vagi are also cut in anesthetized animals, there are prolonged inspiratory spasms that resemble breath-holding. The normal function of the pneumatic center is unknown, but it may play a role in switching between inspiration and expiration.
Regulation of respiratory activity
A rise in the PCO2 or H+ concentration of arterial blood or a drop in its PO2 increases the level of respiratory neuron activity in the medulla, and changes in the opposite direction have a slight inhibitory effect. The effects of variations in blood chemistry on ventilation are mediated via respiratory chemoreceptors—the carotid and aortic bodies and collections of cells in the medulla and elsewhere that are sensitive to changes in the chemistry of the blood. They initiate impulses that stimulate the respiratory center. Superimposed on this basic chemical control of respiration, other afferents provide non-chemical controls that affect breathing in particular situations
Chemical control of breathing
The chemical regulatory mechanisms adjust ventilation in such a way that the alveolar PCO2 is normally held constant, the effects of excess H+ in the blood are combated, and the PO2 is raised when it falls to a potentially dangerous level. The respiratory minute volume is proportional to the metabolic rate, but the link between metabolism and ventilation is CO2, not O2. The receptors in the carotid and aortic bodies are stimulated by a rise in the PCO2 or H+ concentration of arterial blood or a decline in its PO2. After denervation of the carotid chemoreceptors, the response to a drop in PO2 is abolished; the predominant effect of hypoxia after denervation of the carotid bodies is a direct depression of the respiratory center. The response to changes in arterial blood H+ concentration in the pH 7.3–7.5 range is also abolished, although larger changes exert some effect. The response to changes in arterial PCO2, on the other hand, is affected only slightly; it is reduced no more than 30–35%. Feel free to visit to know more about – whealthtips
Summary
Breathing is under both voluntary control (located in the cerebral cortex) and automatic control (driven by pacemaker cells in the medulla). There is a reciprocal innervation to expiratory and inspiratory muscles in that motor neurons supplying expiratory muscles are inactive when motor neurons supplying inspiratory muscles are active, and vice versa.