Renal Function & Micturition
Introduction
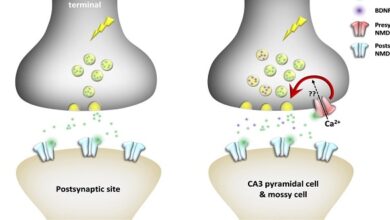
In the kidneys, a fluid that resembles plasma is filtered through the glomerular capillaries into the renal tubules. As this glomerular filtrate passes down the tubules, its volume is reduced and its composition altered by the processes of tubular reabsorption (removal of water and solutes from the tubular fluid) and tubular secretion (secretion of solutes into the tubular fluid) to form the urine that enters the renal pelvis. A comparison of the composition of the plasma and an average urine specimen illustrates the magnitude of some of these changes.
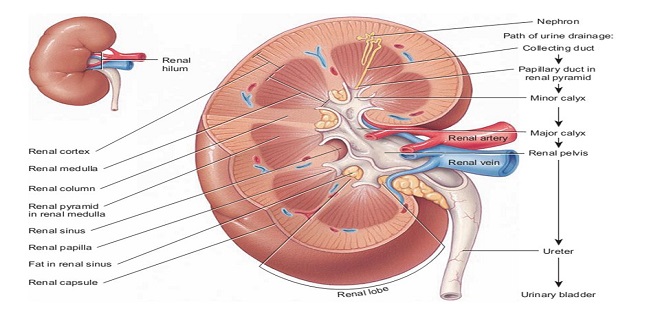
Functional anatomy the nephron
Each individual renal tubule and its glomerulus is a unit (nephron). The size of the kidneys between species varies, as does the number of nephrons they contain. Each human kidney has approximately 1.3 million nephrons. The specific structures of the nephron are shown in a diagrammatic fashion
Lymphatics
The kidneys have an abundant lymphatic supply that drains via the thoracic duct into the venous circulation in the thorax.
Capsule
The renal capsule is thin but tough. If the kidney becomes edematous, the capsule limits the swelling, and the tissue pressure (renal interstitial pressure) rises. This decreases the glomerular filtration rate and is claimed to enhance and prolong anuria in acute renal failure.
Innervation of the renal vessels
The renal nerves travel along the renal blood vessels as they enter the kidney. They contain many postganglionic sympathetic efferent fibers and a few afferent fibers. There also appears to be a cholinergic innervation via the vagus nerve, but its function is uncertain. The sympathetic preganglionic innervation comes primarily from the lower thoracic and upper lumbar segments of the spinal cord, and the cell bodies of the postganglionic neurons are in the sympathetic ganglion chain, in the superior mesenteric ganglion, and along the renal artery. The sympathetic fibers are distributed primarily to the afferent and efferent arterioles, the proximal and distal tubules, and the juxtaglomerular cells. In addition, there is a dense noradrenergic innervation of the thick ascending limb of the loop of Hen
Regulation of the renal blood flow
Norepinephrine (noradrenaline) constricts the renal vessels, with the greatest effect of injected norepinephrine being exerted on the interlobular arteries and the afferent arterioles. Dopamine is made in the kidney and causes renal vasodilation and natriuretic. Angiotensin II exerts a constrictor effect on both the afferent and efferent arterioles. Prostaglandins increase blood flow in the renal cortex and decrease blood flow in the renal medulla. Acetylcholine also produces renal vasodilation. A high-protein diet raises glomerular capillary pressure and increases renal blood flow
Functions of the renal nerves
Stimulation of the renal nerves increases renin secretion by direct action of released norepinephrine on β1-adrenergic receptors on the juxtaglomerular cells and it increases Na+ reabsorption, probably by direct action of norepinephrine on renal tubular cells. The proximal and distal tubules and the thick ascending limb of the loop of Henle are richly innervated. When the renal nerves are stimulated to increasing extents in experimental animals, the first response is an increase in the sensitivity of the juxtaglomerular cells, followed by increased renin secretion, then increased Na+ reabsorption, and finally, at the highest threshold, renal vasoconstriction with decreased glomerular filtration and renal blood flow.
Regional blood flow & oxygen consumption
The main function of the renal cortex is filtration of large volumes of blood through the glomeruli, so it is not surprising that the renal cortical blood flow is relatively great and little oxygen is extracted from the blood. Cortical blood flow is about 5 mL/g of kidney tissue/min (compared with 0.5 mL/g/min in the brain), and the arteriovenous oxygen difference for the whole kidney is only 14 mL/L of blood, compared with 62 mL/L for the brain and 114 mL/L for the heart. The PO2 of the cortex is about 50 mm Hg. On the other hand, maintenance of the osmotic gradient in the medulla requires a relatively low blood flow. It is not surprising, therefore, that the blood flow is about 2.5 mL/g/min in the outer medulla and 0.6 mL/g/min in the inner medulla.
Summary
Plasma enters the kidneys and is filtered in the glomerulus. As the filtrate passes down the nephron and through the tubules its volume is reduced and water and solutes are removed (tubular reabsorption) and waste products are secreted (tubular secretion)